restoreDirect to Implant Breast Reconstruction
restoreDirect to Implant Breast Reconstruction
Procedure
Direct to Implant Reconstruction
Direct to implant reconstruction refers to reconstructing the breast with a breast implant above your chest muscle at the same time of the mastectomy, without requiring a tissue expander. Dr. Spiegel routinely performs direct to implant reconstruction as an outpatient procedure. This means one surgery and you can go home the same day, with no need for a hospital stay.
Historically, implant reconstruction was performed in a staged fashion. During the first stage surgery, a tissue expander was placed to create a space for the breast implant and to establish the breast footprint. Typically, the tissue expander was placed below the chest muscle and expanded gradually in the office. Expansion was required because the breast tissue naturally sits above, not below, the chest muscle so the expander was needed to create a space for the implant. A second stage procedure was required to exchange the tissue expander for an implant. (Read more about the differences between subpectoral and prepectoral breast reconstruction).
Acellular Dermal Matrix
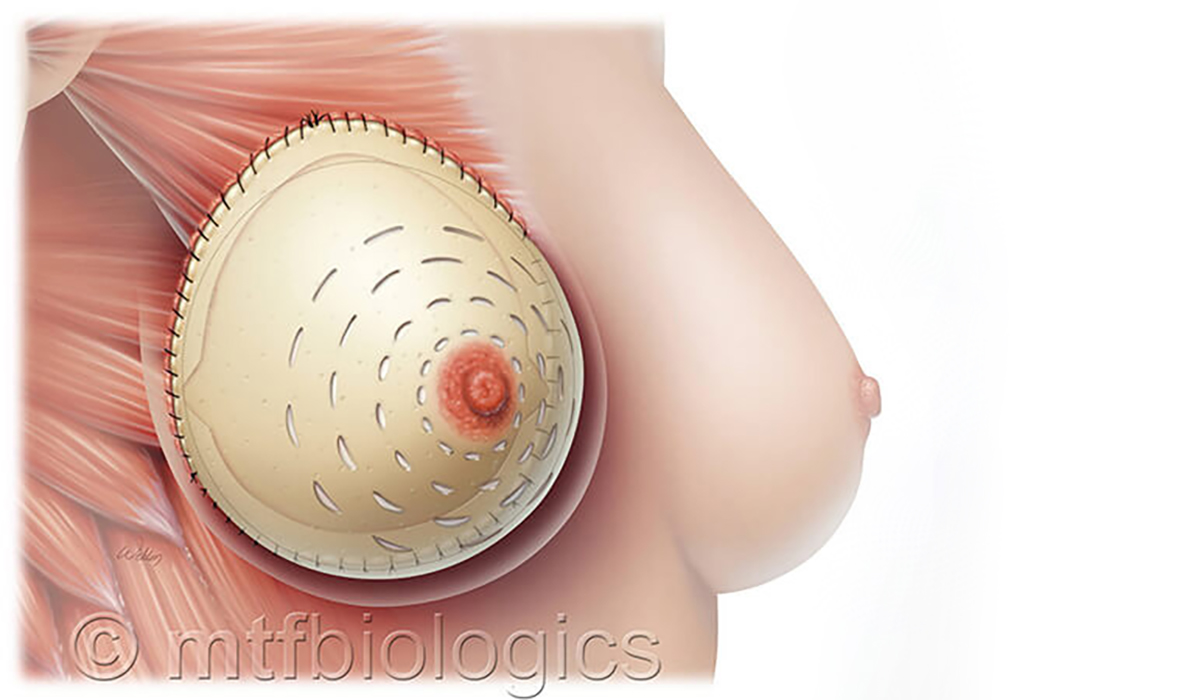
Advances in both surgical technique and technology now allow for the breast to be reconstructed in one surgery above the chest muscle, or using the prepectoral technique. Dr. Spiegel has been on the forefront of prepectoral breast reconstruction and designed a patented acellular dermal matrix that allows for routine direct to implant reconstruction.
Direct to implant reconstruction is possible due to the support and soft tissue coverage of an acellular dermal matrix, which you can think of as an internal bra. The matrix is not a mesh, it is naturally derived of dermis, which is the strength layer of our tissue. The matrix will completely incorporate into your body and strengthen from within, providing the breast implant the support and tissue cover it needs. The acellular dermal matrix also has the added benefit of decreasing the risk of capsular contracture.
What is capsular contracture?
When an implant is placed a capsule, or scar tissue, forms around the implant. This a natural and normal healing process of the body.
Capsular contracture is an abnormal process that happens when this scar tissue hardens and contracts, or tightens, around the implant. This contraction of the capsule applies pressure to the implant and can change the appearance of the breast implant and can cause symptoms such as breast firmness, breast asymmetry, and breast discomfort.
CLASSIFICATION CAPSULAR CONTRACTURE IN BREAST IMPLANTS:
- Grade I:The breast is soft and normal
- Grade II:The breast is less soft than normal, and the implant can be palpated
- Grade III:The breast is firm, the implant can be palpated easily, and an asymmetrical distortion of shape can be appreciated
- Grade IV:The breast is hard, tender, painful, and the shape distortion is pronounced or severe
The cause of capsular contracture is not well understood but theories suggest that a lack of tissue coverage over the implant and infection can play a role in the development of capsular contracture. Acellular dermal matrixes have been found to be protective and reduce the risk of developing capsular contracture.
The acellular dermal matrix used is a patented technology designed specifically to create a natural breast shape with preferential projection in the center of the breast under the nipple.
The design of the matrix allows Dr. Spiegel to tailor the breast reconstruction to your specific breast footprint. The matrix is sewn into place with stitches to set the footprint of your breast, which will absorb as the matrix incorporates into your body. The results in a soft, natural, and beautiful reconstructed breast.
The Incision
One incision is made to each breast. The location of the breast incision varies patient to patient. In the case of a nipple sparing mastectomy, the incision will be hidden in the breast crease and results in the look of a completely unoperated breast.
Factors considered when determining incision placement include the type of mastectomy the patient is having, the incision the general surgeon will be using to complete the mastectomy, and specific past surgical history.
Please visit the Breast Cancer Surgery page for more information regarding mastectomy options.
Candidates
You may be a candidate for DIRECT TO IMPLANT reconstruction if you are in good general health and:
- You are scheduled to have a nipple sparing mastectomy due to a new breast cancer diagnosis or you are considering a prophylactic mastectomy.
- You desire a natural look and feel to the breast with fewer surgeries and faster recovery
- You have minimal excess fatty tissue present to reconstruct the breast with your own tissue and/or you do not want to add additional scars to your body
- You had a previous breast reconstruction with implants placed below your muscle and are experiencing breast discomfort or pectoral animation and would like the implants converted to be placed above your muscle
- You have a complex health history that requires a simpler procedure with shorter time under general anesthesia
Things to consider:
- This reconstruction may require more than one procedure and direct to implant reconstruction is not guaranteed.
- When possible, we prefer to place an implant directly, but there are multiple factors that effect this decision including type and location of cancer, type of mastectomy, and your desired breast size
- A tissue expander is always ordered and available as a backup option. A tissue expander would be placed if it is determined in the operating room that it is not safe to proceed with direct to implant reconstruction.
- Although direct to implant can be a one stage surgery, most patients benefit from a second stage surgery of fat grafting to camouflage the breast implant and smooth out any mastectomy irregularities. This procedure will focus on refining the breast shape.
Benefits
There are multiple benefits of implant based reconstruction including:
- Simple procedure with little downtime
- Direct to implant reconstruction is an outpatient procedure that does not require a hospital stay. Most patients can return to light activity four weeks after surgery.
- Natural feel and appearance of the breast
- Prepectoral breast reconstruction, especially when combined with a nipple sparing mastectomy, can result in the appearance of a natural, unoperated breast
- Maintain breast shape during radiation therapy
- Implant based reconstruction is a great option to maintain the shape and contour of the breast during radiation therapy, if required for your cancer treatment
Risks
Breast implants are FDA-approved devices and are an important option for breast reconstruction.
Complications of implant based breast reconstruction may include infection, seroma (fluid developing around the breast implant), capsular contracture (contracted scar tissue causing breast discomfort and firmness), and implant rupture. These complications are reduced by surgical technique, the placement of breast drains, intraoperative antibiotics, patient activity restrictions, and post surgical oral antibiotics.
Patient safety is our number one concern. Dr. Spiegel is dedicated to patient advocacy, advances in breast surgery, and medical safety. For more information and resources regarding breast implant safety and for information regarding BIA-ALCL please visit the Breast Implant Safety information page.

Recovery
Implant reconstruction is typically an outpatient procedure, so you will go home the same day as your surgery. You will be sent home with drains. Two drains are placed to each operated breast. Drains are typically removed within 2-3 weeks, depending on the drain output.
Your arm range of motion will be restricted during your initial recovery. We ask that you do not perform repetitive motions with the arms or household chores for the first few weeks after surgery. Limiting your arm range of motion decreases the amount of fluid that accumulates are the breast implant, allowing for drains to be removed sooner.
One of the main factors in healing after implant reconstruction is decreasing fluid accumulation around the breast implant. This leads to a quicker recovery and decreases the risk of infection. Most patients will be released to full arm range of motion at 3 weeks and can return to light daily activities 4 weeks after surgery. Most patients can resume all activities without restrictions, including lifting, at 2-3 months.
For a detailed layout of what to expect after your implant reconstruction please click here for the Implant Week by Week Guide.

Results
Advances in both mastectomy technique and implant based reconstruction have allowed for excellent short and long term results. Prepectoral implant placement has allowed for a natural contour, shape, and feel to the breast. When combined with a nipple sparing mastectomy, Dr. Spiegel is able to reconstruct the breast to the extent where patient’s note they feel and look as though they have not been operated on.
Advances in silicone breast implant technology have lowered rates of implant rupture and it is not necessary to regularly exchange an intact breast implant in a patient that is doing well with no symptoms or concerns. Maintenance of silicone breast implants includes monitoring the implants with a breast MRI every 3 years to ensure the implants are intact.
